NZ Media Releases
Health expert answers common Covid-19 vaccine questions
Dr Natalie Gray
Public Health Physician
As part of a Q+A session with ANZ staff, Australian public health physician Dr Natalie Gray answered some of the most common questions about the Pfizer Covid-19 vaccine, and cleared up some misconceptions.

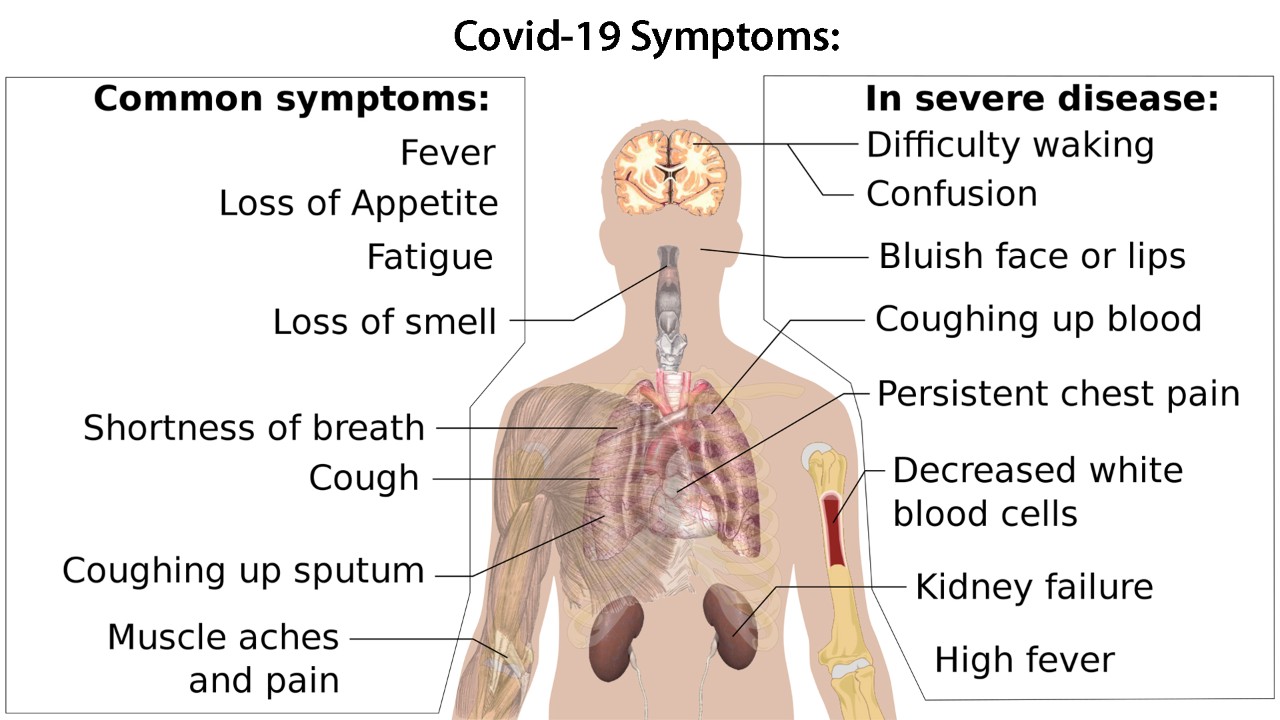
What exactly is the Delta variant of Covid-19, and why is it worse than the original?
The Delta variant has become the dominant type of Covid-19 circulating worldwide, largely because of a mutation this strain went through in its spike proteins. Everybody knows what the Covid virus looks like now – it’s a ball shape with lots of little spikes coming off – and those are the spike proteins.
The mutation which created Delta makes those spike proteins stickier – they attach more strongly to our lungs and that means we need to breathe in less of the virus to become infected, and once we become infected, Delta is able to replicate more quickly, increasing the amount of virus in our body.
The original virus, which first surfaced in Wuhan, China, had a reproduction rate in an unvaccinated population of about 2.5 – every infected person, on average, infects 2.5 other people. The Alpha variant, which surfaced in the UK, had a rate of between 4-5. Delta is about 60% more transmissible than Alpha, so its reproduction rate is between 5-8, although in some studies it’s been shown to be as high as 9 or 11.
"When someone comes home with Delta, pretty much everyone in the family gets infected, assuming they’re not vaccinated. If people are not wearing masks and working closely together, whole workplaces can get infected. The Delta variant is so much more infectious than the original."
- Dr Natalie Gray, Public Health Physician
If I speak or sing or cough or sneeze – droplets come out of the nose and mouth. Most of the droplets fall to the ground within about two metres, so you’d need to be quite close to someone to breathe them in. That’s where the two-metre social distancing rule came from.
But with Delta, you get more virus in the small particles that are expelled, which we call aerosol, and those stay in the air for a longer period of time, and can travel further from the infected person. So we know now that you don’t have to cough right in someone’s face to transmit Delta – a person in a room can expel those aerosols, leave the room, and another person coming in can breathe those in and become infected. This is called airborne transmission.
It’s also possible to contract Covid by touching a contaminated surface and then touching your face, but that is much, much less common than we were originally concerned about – the vast majority of infections occur through droplets and aerosols.
We also now know that the Delta variant causes more serious disease than previous variants. An unvaccinated person infected with Delta is about twice as likely to need intensive care treatment, and 1.5 times as likely to die, as someone infected with the Alpha variant.
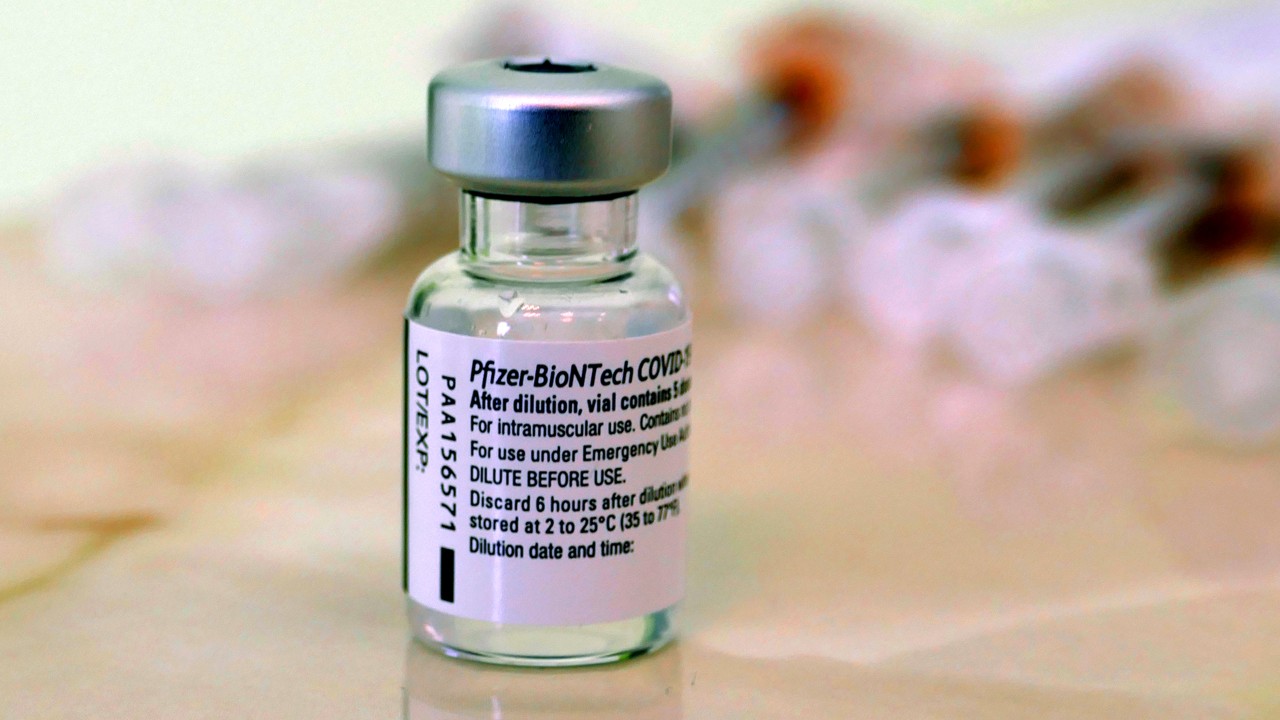
How effective is the Pfizer Covid vaccine?
Using data from the UK real world studies on the Pfizer vaccine during 2021, we find there is evidence of some protection after one dose – about a 33 per cent protection from infection, and about 70 per cent protection from serious disease – we use hospitalisation as the marker for serious disease.
After two doses of Pfizer, somewhere between three and six weeks apart, protection goes up much higher. Protection from infection goes up to about 72 per cent, and protection against serious illness goes up to about 96 per cent.
Furthermore, protection against actually dying from Covid is very high – if you have no underlying medical conditions, it’s about 99 per cent, and in some studies, as high as 99.8 per cent. For people with complex medical problems and who are in the older age group, two doses give about 90 per cent protection from death.
The other thing we know about this vaccine is that it reduces how infectious you are – so even if people become infected, they carry virus within their body for a shorter period of time (about 6 days compared with 14-16 days for unvaccinated people) and they are less likely to pass it on to other people – data suggests vaccinated people transmit the virus half as much as unvaccinated people.
Among vaccinated people, we are seeing time and time again that they will either have no symptoms at all, or will have very mild symptoms similar to those annoying winter respiratory illnesses we all get.
If someone contracts Covid-19, what treatments are currently available?
For people who are mildly or moderately unwell, with no underlying medical conditions, essentially you’re looking at the same treatments you would use if you had the flu – paracetamol, drinking lots of fluids and rest.
In Australia, if you fall into a high risk group because of underlying health factors, there is a newly-approved experimental monoclonal antibody treatment available called sotrovimab. This drug has been shown to reduce hospitalisation or death by 70-80 per cent in adults with mild to moderate Covid-19, who are at risk of developing severe Covid-19. It needs to be given intravenously (through your veins) and so can only be administered in a health facility.
Monoclonal antibody treatments are essentially antibodies against Covid-19 produced in a lab, and help to fire up your immune system to fight the virus.
In New Zealand, MedSafe has not yet approved sotrovimab for use, but several experts have argued that it should be considered in the very near future.
Covid-19 patients in hospital are often administered oxygen through a face mask, but if their need becomes greater, they will then be moved into intensive care to be put on a respirator machine. These machines work by putting tubes into your lungs through the mouth, and delivering oxygen into them directly – essentially breathing for you.
If someone has had Covid-19 and recovered, is their immunity greater than that provided by the vaccine?
When people are exposed to a virus naturally, the development of their immunity to it afterwards is highly variable. Some people will get good long term protection, some will have good protection for a shorter period of time, and some will get almost no protection from subsequent infections at all.
We do know that, among all of those people, your immune response will much stronger, and much more long-lived if you get a Covid-19 vaccine after being infected naturally.
In vaccines, people receive a uniform dosage each time, and you get a much more even level of antibodies compared with a natural infection, which may severe, or have no symptoms, depending on the viral load.
So in short, natural immunity is a good start, and if you go on to get a vaccination, you’ll get good, long-lasting protection.
Are there any side effects from the Pfizer vaccine that are not treatable?
There are generally three time frames, when it comes to vaccine side effects – immediate, short term and long term.
Immediate side effects include being allergic to the shot, called anaphylaxis, and medical staff delivering the vaccines are highly trained to deal with this, if it takes place. That’s why people are required to wait around after the shot – to ensure they don’t have an allergic reaction, and treat it if it does take place.
Short term, within the first 72 hours after the vaccine, you get a big boost in your antibody response, which generally comes along with a sore arm, headache, fevers and aches and pains.
If you get none of those side effects at all – it doesn’t mean the vaccine isn’t working, it’s just that some people are more susceptible to those effects.
Long term, within the next 6-8 weeks, there is one extremely rare side effect – inflammation of the heart. This is either myocarditis (inflammation of the heart itself), pericarditis (inflammation of the fluid filled sac around your heart), or a combination of both (myopericarditis).
These conditions occur normally among the general population for a variety of reasons, at a very, very low rate – in young men it’s about 37 cases per million, and in young women it’s about 16 per million.
What we’re finding with the Pfizer vaccine, is that there’s a very, very small increase in the number of cases of those, above the usual ‘background’ rate.
More research is being done to understand this increase, but from the 100’s of millions of doses of Pfizer administered across Europe and the US, scientists have discerned that the approximate risk of getting myocarditis or pericarditis from the Pfizer jab, across all ages range, is about 1-2 in a million, which is about the same odds as getting struck by lightning this year.
Younger people appear to be more at risk, and if you’re under 40, the odds are about 1 in 125,000, which is still extremely small – about a quarter of the risk of you dying in a car accident this year.
Both conditions are very treatable. Most people with one of those conditions will go to hospital and be treated with steroids, while being monitored, and will generally recover completely within a week.
Beyond eight weeks, following the vaccine, there has never been a side effect attributed - to any vaccine. After eight weeks, your immune system goes back to baseline, and the vaccine has long since been eliminated from your body. The only thing that persists is the memory, within your immune system, of how to fight Covid by producing the right antibodies, if it re-emerges.
How long does the vaccine stay within your body, and can you shed it through your pores?
The Pfizer vaccine normally stays in your body for between 48-72 hours.
The Pfizer vaccine uses mRNA technology. A set of genetic instructions is delivered to your body to produce a certain part of the Covid-19 virus – the spike protein.
Your muscle cells (which is where the vaccine is injected) rapidly go about manufacturing these proteins, but soon afterwards, the immune system recognizes them as foreign bodies, and begins producing antibodies to eliminate them.
Meanwhile, the mRNA instructions, as well as the small molecule of fat they are delivered inside, and the sugars and salts used to stabilise the vaccine, become useless after a spike protein is made, and are eliminated from the body as waste.
None of the Covid vaccines contain any live virus – so it is not possible for you to shed any virus after being vaccinated.
What about the vaccine’s effect on pregnant women, and on fertility?
The Pfizer vaccine has been highly studied in relation to pregnancy – women across all stages of pregnancy have been studied. Those studies have shown both that the vaccine is as effective in pregnant as in non-pregnant women, and that there are no side effects above and beyond those in the general population.
While no component of the vaccine passes to the baby, a mother vaccinated during pregnancy does pass on some immunity to her baby when it is born, which is good news, because babies under the age of six months will likely never be able to be vaccinated against Covid.
Pregnant women are highly encouraged to get vaccinated, because pregnancy puts them at a high risk of serious Covid-19 effects, if they get it. They’re more likely to require hospital treatment, more likely to require a ventilator, and are at higher risk of a pre-term birth.
"There is no scientific basis for any vaccine-related side effects beyond the 8-week mark, following vaccination, as your body has essentially returned to the state it was before you were vaccinated – but with a stronger immune system against Covid."
- Dr Natalie Gray, Public Health Physician
Misinformation about the effects of the vaccine on pregnant women has come from various sources, including one completely unfounded theory that Covid-19’s spike protein looked similar to another protein used by the body during fetal development.
Subsequent studies have shown that theory has absolutely no scientific basis. The proteins do not act in the same way, and in fact don’t even look particularly similar - they are entirely unrelated.
There is no evidence, at all, that any Covid-19 vaccines affect fertility for either women or men in either the short, or long term.
Some women have reported an early, late, or heavier menstrual period following vaccination, but that is considered to be a normal side effect of the initial immune response, much the same as aches and pains or a headache.
The endometrium – the lining of the uterus – contains immune cells, so it is involved in the whole-of-body immune response. But that does not mean an effect on fertility – it means the whole of your body is responding to the challenge to the immune system.
How about teenagers – those aged 12-16?
The Pfizer vaccine has been approved for people over the age of 12, and studies have been carried out showing that the vaccine is equally effective, and equally safe in this age group – possibly even more effective, since they have better immune systems.
Australian data does show a slightly increased risk of myocarditis and pericarditis in teenage boys, compared with the rest of the population, but that risk remains incredibly low at about 5.2 cases per 100,000, and the condition is treatable.
What does science say about the length between Pfizer doses?
Your Pfizer vaccination will be equally effective in the shorter term, regardless of the interval between the two doses.
There’s some evidence now that the Pfizer vaccine may have longer-term protection if you get the two doses with six weeks in between, compared to a shorter interval.
There is also evidence that a third dose, six months after your second dose, is of benefit which is why countries that have achieved high rates of double dose protection are now looking at rolling out a third dose ‘booster’.
RELATED ARTICLES
NZ Business
Fiji's Covid-19 outbreak prompts a new way of leading
NZ Media Releases